Adenoidid is often described as a simple infection of the adenoids that should resolve with medication or time. Yet for many children—and even some adults—adenoid inflammation becomes chronic, recurrent, or resistant to treatment. Parents are left wondering why symptoms never fully disappear, and patients continue to struggle with nasal blockage, mouth breathing, snoring, or repeated infections.
The truth is that the most common explanations only scratch the surface. Behind recurring or persistent adenoidid are hidden causes that involve the immune system, microbiome imbalance, environmental exposure, and silent inflammatory mechanisms that standard treatments fail to address.
This article explains those hidden causes in a clear, practical way, helping you understand why adenoidid persists, why antibiotics often fail, and what actually drives long-term adenoid inflammation.
Understanding Adenoidid Beyond Infection
| Aspect | Acute Adenoidid | Chronic Adenoidid (Hidden Causes) |
|---|---|---|
| Primary trigger | Bacterial or viral infection | Immune dysfunction, biofilms, allergies |
| Duration | Short-term | Long-lasting or recurrent |
| Response to antibiotics | Usually effective | Often ineffective |
| Presence of fever | Common | Rare or absent |
| Tissue state | Temporarily inflamed | Persistently swollen |
| Diagnosis difficulty | Easy | Immune dysfunction, biofilms, and allergies |
Adenoidid refers to inflammation of the adenoids, also known as the pharyngeal tonsils, located in the upper part of the throat behind the nose (the nasopharynx). These lymphoid tissues are part of the immune system and act as a first-line defense against airborne pathogens.
Adenoidid vs Adenoid Hypertrophy
A key reason adenoid problems are misunderstood is confusion between two related conditions:
- Adenoidid: active inflammation, often recurrent or chronic
- Adenoid hypertrophy: persistent enlargement of adenoid tissue, sometimes without active infection
Enlarged adenoids are not always infected. In many cases, silent inflammation or immune overstimulation keeps the tissue swollen long after an infection has passed.
Why Acute Causes Don’t Explain Chronic Cases
A single bacterial or viral infection rarely explains:
- persistent adenoid swelling
- repeated adenoid infections
- symptoms lasting months or years
Chronic adenoid disease follows a different biological pathway—one driven by immune response dysfunction rather than ongoing acute infection.
Immune System Dysfunction as a Root Cause
Mucosal Immunity Failure
The adenoids are part of the mucosal immune system, which relies heavily on IgA immune response to neutralize pathogens. When this system becomes dysregulated, the adenoids may overreact to harmless stimuli.
This leads to:
- lymphoid tissue overgrowth
- chronic inflammatory mediators are released
- persistent adenoid swelling without infection
In simple terms, the immune system gets “stuck in defense mode.”
Chronic Inflammatory Response Loops
Once inflammation becomes chronic, the body enters a self-sustaining cycle:
- Initial infection or irritation
- Inflammatory cytokines released
- Tissue swelling narrows the airway
- Reduced drainage and airflow
- Ongoing irritation → more inflammation
This chronic inflammatory cycle explains why adenoiditis keeps returning even after treatment.
Hidden Infectious Triggers Most People Miss
| Hidden Trigger | How It Affects Adenoids | Why It’s Hard to Detect |
|---|---|---|
| Bacterial biofilms | Protect bacteria from treatment | Not visible in routine tests |
| Viral persistence | Keeps immune system activated | No active infection signs |
| Subclinical infection | Causes silent inflammation | No fever or pain |
| Antibiotic resistance | Leads to repeated relapse | Symptoms temporarily improve |
Bacterial Biofilms in Adenoids
One of the most overlooked causes of chronic adenoidid is bacterial biofilm formation.
Biofilms are structured communities of bacteria that:
- attach to the adenoid tissue
- hide behind a protective matrix
- resist antibiotics and immune attack
This creates subclinical adenoid infection—bacteria are present, but not actively causing fever or pain. As a result, tests may appear normal while inflammation continues.
Why antibiotics often fail:
Antibiotics kill free-floating bacteria, not bacteria protected inside biofilms. This explains antibiotic-resistant adenoid biofilms and frequent relapse.
Viral Persistence and Latent Infections
Certain viruses can remain dormant within lymphoid tissue. This viral persistence in adenoids acts as a constant immune trigger, even without active illness.
This viral reservoir theory explains:
- recurrent inflammation without acute symptoms
- adenoid swelling without bacterial growth
- Immune memory dysfunction in adenoids
Also read: Is Aspartame Safe? How It Affects Metabolism, Brain, and Health
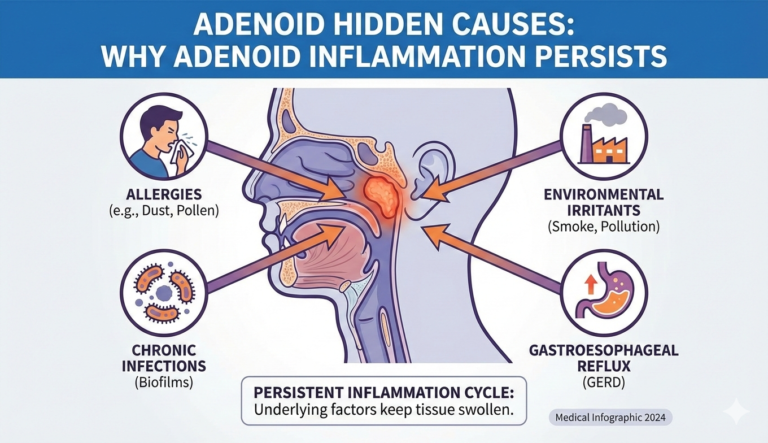
Non-Infectious Hidden Causes of Adenoidid
| Non-Infectious Cause | Mechanism | Commonly Overlooked Because |
|---|---|---|
| Allergic inflammation | Immune overreaction | No infection present |
| Acid reflux (GERD) | Acid irritates nasopharynx | No digestive symptoms |
| Air pollution | Chronic mucosal irritation | Gradual symptom onset |
| Indoor toxins | Immune overstimulation | Seen as environmental “normal” |
Allergic Inflammation Without Infection
Allergic rhinitis doesn’t just affect the nose—it also impacts the adenoids. Chronic exposure to allergens leads to:
- adenoid allergic reaction pathways
- non-infectious adenoidid
- nasal obstruction, immune-related causes
In these cases, inflammation occurs without bacteria or viruses, making antibiotics ineffective.
Acid Reflux and Nasopharyngeal Irritation
Gastroesophageal reflux disease (GERD) is a frequently missed cause of adenoid inflammation. Acid vapors can reach the nasopharynx, irritating adenoid tissue repeatedly.
This reflux-induced nasopharyngeal inflammation:
- causes chronic irritation factors
- worsens nighttime symptoms
- contributes to sleep-disordered breathing
Children may not complain of heartburn, making this cause easy to miss.
Environmental Pollutants and Air Quality
Long-term exposure to:
- air pollution
- cigarette smoke
- indoor toxins
can trigger chronic upper airway inflammation. The adenoids respond by enlarging, even in the absence of infection.
This environmental toxin nasal exposure effect is increasingly common in urban settings.
Microbiome Imbalance and Adenoid Disease
Disrupted Nasopharyngeal Flora
Healthy adenoids contain a balanced microbial ecosystem. When this adenoid microbiome imbalance occurs, harmful bacteria dominate and beneficial microbes decline.
This imbalance:
- promotes chronic inflammation
- supports biofilm development
- increases recurrence risk
Why Antibiotics Make It Worse
Repeated antibiotic use can:
- Disrupt beneficial bacteria
- promote resistant strains
- worsen inflammatory relapse cycles
This is why children with frequent antibiotic exposure often develop chronic adenoid disease pathophysiology.
Structural and Genetic Contributors
| Diagnostic Method | What It Reveals | Why It’s Important |
|---|---|---|
| Nasal endoscopy | Adenoid size and inflammation | Direct visualization |
| Symptom pattern analysis | Chronic vs acute signs | Avoids misdiagnosis |
| Allergy assessment | Non-infectious triggers | Prevents unnecessary antibiotics |
| Treatment response tracking | Hidden resistance patterns | Guides long-term care |
Anatomical Narrowing Effects
Some children naturally have:
- narrow nasopharyngeal anatomy
- obstructive nasal pathology
Even mild inflammation can cause significant blockage, leading to persistent symptoms.
Genetic Immune Sensitivity
Certain individuals inherit:
- heightened immune reactivity
- Immune tolerance failure in adenoids
Their immune system responds excessively to normal exposures, leading to silent adenoid hypertrophy.
Why Adenoiditis Is Commonly Misdiagnosed
Overlap With Sinus and Tonsil Disorders
Adenoid symptoms mimic:
- chronic sinus inflammation
- tonsillitis
- allergic rhinitis
As a result, adenoid inflammation misdiagnosis patterns are common.
Silent Symptoms Parents Miss
Adenoidid often exists without:
- fever
- sore throat
- obvious pain
Instead, signs include:
- mouth breathing
- snoring
- nasal speech
- poor sleep quality
This silent presentation delays diagnosis.
Long-Term Risks of Untreated Hidden Causes
Sleep and Breathing Disorders
Enlarged adenoids contribute to:
- sleep-disordered breathing
- pediatric obstructive symptoms
- behavioral and learning issues
Recurrent ENT Infections
Chronic adenoid inflammation becomes a reservoir for pathogens, increasing:
- ear infections
- sinus infections
- chronic nasal obstruction
Identifying Hidden Causes Clinically
Diagnostic Imaging and Endoscopy
Nasal endoscopy allows direct visualization of:
- adenoid size
- inflammation patterns
- mucus and biofilm presence
This is far more accurate than symptom-based diagnosis alone.
When to Consider Surgical Evaluation
Adenoidectomy may be considered when:
- conservative treatments fail
- biofilm-related disease persists
- breathing or sleep is affected
Surgery removes the inflammatory source, breaking the immune overload cycle.
Frequently Asked Questions About Adenoidid Hidden Causes
What are the hidden causes of adenoidid?
Immune dysfunction, bacterial biofilms, viral persistence, allergies, reflux, microbiome imbalance, and environmental exposure.
Why does adenoidid keep coming back?
Because chronic inflammation, not active infection, is often the driving force.
Can adenoidid exist without fever or pain?
Yes. Subclinical and non-infectious adenoidid are common.
Why doesn’t adenoidid respond to antibiotics?
Biofilms, viral latency, and immune-mediated inflammation are antibiotic-resistant.
Can adults have adenoidid?
Yes, though it is less common, often linked to immune or environmental factors.